Your Pregnancy

Preparing for birth
 Now days there are so many wonderful resources out there to help prepare you for birth. Just remember knowledge is POWER!! The goal of a preparatory class is to empower you to pursue the kind of birth that’s right for you and your partner.
Now days there are so many wonderful resources out there to help prepare you for birth. Just remember knowledge is POWER!! The goal of a preparatory class is to empower you to pursue the kind of birth that’s right for you and your partner.
The more you know about the birthing process, the more you will realize just how amazing your body is, which, will lead to less fear and positive vibes during labor. These classes will also help you understand the rhythm of pushing and the intensity of transition. Remember you are STRONG and your body was meant to birth your beautfiul baby.
Find a birthing method that is right for you and your partner, one that fits y our personal learning style, and goals. Remember, there is not one right way to have a baby! Some classes that provide valuable education and birthing techniques are listed below:
our personal learning style, and goals. Remember, there is not one right way to have a baby! Some classes that provide valuable education and birthing techniques are listed below:
- Lamaze
- Bradley Method
- Hypnobirthing
- Hypnobabies
- Informed Beginnings
- Birthing from Within
- Breastfeeding Class
Most of the classes listed above provide breastfeeding education. It is important to note the importance of breastfeeding. In my experience, I felt like no one warned me how painful breastfeeding can be, especially in the beginning.
Ask for help! Ask your midwife about local resources in your community to help give you support if you are having trouble. Most insurance companies will cover the cost of a breast pump so take advantage. Whatever you do, don’t give up! It’s hard in the beginning but it gets better and better. In just a few short weeks, your baby will be nursing like a pro. Research confirms that the best way to feed your baby is to breastfeed; formula feeding is a choice that should be best reserved for situations of necessity [1] . Enjoy this time you spend together with your baby, it will help you bond.
If I could stress one thing it would be the importance of having a birth plan and knowing what is important to YOU. It is important to communicate this with your midwife so he or she can do everything is their power to ensure your wishes are granted. Just remember your midwife is cheering for you and wants you to have a positive experience. Click MY BIRTH PLANfor an example birth plan.
Resources
1.https://www.cdc.gov/breastfeeding/recommendations/
2.http://www.lamaze.org/FindALamazeChildbirthClass
3.http://www.bradleybirth.com/
4.http://us. hypnobirthing.com/
6.http://www.birthingfromwithin.com/
7.http://www.informedbeginnings.org/
8.http://www.firstlatch.net/index.php?option=com_content&view=article&layout=edit&id=25

Induction
 The first thing a woman does after she gets a positive pregnancy test is fantasize about the day the baby will be born. Most of us wish that the baby will make it to term but will be born early, somewhere between 37-39 weeks gestation to be exact. Pregnancy can seem to last forever and the excitement you have to meet your little one can be overwhelming. Many women become miserable towards the end of their pregnancy and will do anything to be “done.” It’s important to remember that in hindsight your pregnancy will go fast and your little one will be in your arms before you know it.
The first thing a woman does after she gets a positive pregnancy test is fantasize about the day the baby will be born. Most of us wish that the baby will make it to term but will be born early, somewhere between 37-39 weeks gestation to be exact. Pregnancy can seem to last forever and the excitement you have to meet your little one can be overwhelming. Many women become miserable towards the end of their pregnancy and will do anything to be “done.” It’s important to remember that in hindsight your pregnancy will go fast and your little one will be in your arms before you know it.
“To all the mamas who are waiting patiently (and sometimes anxiously) for labor to begin: remember that this is your first act of selflessness as a mother. There will be many more. But for now, this acceptance of your child’s unique journey, this willingness to trust your baby, will set the tone for your future relationships.” -Lauralyn Curtis
 Sometimes medical induction is necessary to prevent risks from complications that arise during pregnancy. Induction of labor should be offered only for certain medical complications that are supported by scientific evidence and prove the benefit outweighs the risk of induction [1]. These medical indications include disorders like gestational diabetes, gestational hypertension, intrauterine growth restrictions, and cholestasis [2]. Your midwife will communicate the current evidence-based guidelines and provide counseling in helping you make the right decision for you and your partner. Through education and valuable discussions with your midwife, she or he can assist in helping you make an informed decisions regarding induction.
Sometimes medical induction is necessary to prevent risks from complications that arise during pregnancy. Induction of labor should be offered only for certain medical complications that are supported by scientific evidence and prove the benefit outweighs the risk of induction [1]. These medical indications include disorders like gestational diabetes, gestational hypertension, intrauterine growth restrictions, and cholestasis [2]. Your midwife will communicate the current evidence-based guidelines and provide counseling in helping you make the right decision for you and your partner. Through education and valuable discussions with your midwife, she or he can assist in helping you make an informed decisions regarding induction.
Midwives strongly support the normal physiologic process of birth. We believe that spontaneous labor offers substantial benefit to the mother and her newborn. Disruption of the normal physiologic process of birth without an evidence-based medical indication represents a risk for potential harm[1]. Elective induction has been noted as contributing to late pre-term births and should never be offered to any woman prior to 39 weeks gestation. Elective induction before 41 weeks gestation can increase the chance of having cesarean if the cervix hasn’t softened or there is minimal dilation [1].
The goal of a midwife is to empower women to have normal physiologic labor–this is characterized by spontaneous onset and progression of labor. Induction of labor interferes with the normal physiological processes of spontaneous labor; the full extent of the disruption is not well known [1]. Research related to the long term effects of induction is emerging but is still insufficient to determine the full impact of newborn effects. Current studies are finding disruption in fetal brain development and increased risk for Autism Spectrum Disorders and behavioral concerns. Evidence also suggests that some critical processes, such as lactogenesis, attachment, and parenting are interrupted by induction of labor [1].
The decision to induce labor requires consideration of the potential for harm verse benefit, including short and long-term complications for the woman and her baby. Ask your midwife to discuss these risks with you. Remember midwives promote choice—you always have CHOICES. Your decisions and requests are always valued so never hesitate to talk openly with your midwife.
Induction Methods
 If induction is recommended it’s important to request to have cervical ripening agents if your cervix is unfavorable. Unfavorable means your cervix is not dilated or barley dilated, firm, and still high in your vagina. Cervical ripening agents decrease the chance of needing a cesarean. Cervical ripening agents can take between 4-24 hours or even longer in some cases. Cervical ripening agents include the following:
If induction is recommended it’s important to request to have cervical ripening agents if your cervix is unfavorable. Unfavorable means your cervix is not dilated or barley dilated, firm, and still high in your vagina. Cervical ripening agents decrease the chance of needing a cesarean. Cervical ripening agents can take between 4-24 hours or even longer in some cases. Cervical ripening agents include the following:
- Cervidil: This medication is a prostaglandin that is placed in your vagina for 12 hours—it releases 0.3mg of medication an hour. It kind of looks like a small tampon with a string on it. This medication works by softening your cervix (the opening of your uterus) and helps with dilation. One benefit of this medication is you can take it out at anytime. One risk is that this medication can cause your uterus to start contracting to frequently, the good news is if this happens it can quickly be removed. A downfall is that this medication works for over 12 hours, so it can take a long time.
- Cytotec: This is another prostaglandin medication used to soften your cervix and encourage dilation. This medication is not FDA approved for cervical ripening but is standardly used throughout the US as a cervical ripening medication for induction. It can be dosed every 4 hours for 3 doses—you can place it in your cheek and it will dissolve, you can swallow it, or it can be inserted into your vagina. This medication has the same risk of Cervidil in causing frequent contractions and it cannot be removed once administered. The benefit is that this medication only takes 4 hours but it is possible that you will need another dose or two.
- Low-dose Pitocin: Pitocin also known as “Oxytocin,” is a synthetic hormone of a naturally occurring hormone we normally produce in our brain. This medication is given in a IV. This hormone helps the uterus contract effectively during labor. Low-dose Pitocin can be used as a cervical ripening agent. This means that the dose of Pitocin will never go above 4 milliunits per hour. The side effects of this medication are that the baby will not tolerate the medication or it might cause contractions too frequently. This is rare when administered at such a low level. The good news is it can quickly be turned off.
- Foley balloon (Cooks catheter): This is the most common method of mechanically dilating the cervix [3]. Your midwife will use a speculum or his or her fingers to insert a small balloon into your cervix; she will then insert some sterile water to inflate the balloon, about 30 cc’s. This will put mild tension on your cervix. The balloon will fall out on it’s own when your cervix dilates to a 3 cm—this usually takes between 6-12 hrs. The benefit of this procedure is that it ripens the cervix in a natural way using no synthetic hormones. This is the most “natural way” to ripen the cervix. The risk is that it can cause your bag of water to break and in rare cases the cord can prolapse. This is uncommon and rarely occurs but it is a risk to be aware of. The procedure can also be a little uncomfortable and cause some cramping but once it is in place the discomfort usually goes away.
When you start active labor there are other methods to help encourage continual dilation of your cervix and adequate uterine contractions to promote the birth of your baby. These two methods are listed below.
- Breaking bag of water: Your midwife will use a tool called an “amniohook” to break your bag of water. This can be uncomfortable but it is not a painful procedure. This helps the baby engage in the pelvis and put pressure on the cervix increasing dilation + progression of labor. The risk of this procedure is that it can cause the baby to become malpositioned, the cord can prolapse, and there is always an increased risk of infection if your bag of water is broken for a long period. This method of induction can shorten the period of labor by 2 hours or more [1].
- Pitocin: Pitocin also known as “Oxytocin,” is a synthetic hormone of a naturally occurring hormone we normally produce in our brain to stimulate labor. This hormone helps the uterus contract effectively during labor. This hormone can also help the uterus contract down to its prepregnancy size after you delivery your baby. This medication is administered IV during labor and your baby’s heart rate is continuously monitored to ensure they are tolerating the medication. Risks of this medication include that your baby will not tolerate the medication, it can cause your uterus to contract too much, your blood pressure to drop, and there is a chance of increased blood loss after the delivery of your baby. Your midwife and nurses will be monitoring your baby closely to ensure you and your baby are tolerating this medication. This is a very common medication and used frequently on the labor & delivery unit.
Expected Time Frame
Induction can take anywhere from 6 to 72 hours or longer. Usually, women who are having a baby for the first time have a longer induction than women who have already had a baby. The most important thing to remember is that it can take time, so have patience and bring some movies to watch or games to play with your husband while you wait for active labor to begin. Your midwife will be by your side every step of the way—she or he will give you thorough education regarding risk, benefits, and alternative options. Just remember you always have CHOICES.
Resources
2.http://www.acog.org/Womens-Health/Labor-Induction
3.http://transform.childbirthconnection.org/2013/02/choosing-wisely/

Postpartum Depression
Approximately 85% of women will experience a mood disorder before, during, or after pregnancy [1].  Postpartum depression is a disorder that causes an overwhelming feeling of anxiety and/or depression after you give birth to your baby. Many women wonder what causes postpartum depression and if there is anything they can do to prevent it. Postpartum depression does not occur because of something a mother does or does not do. The exact causes of postpartum depression are not well known—it is thought that it is caused by a combination of physical and emotional factors [2].
Postpartum depression is a disorder that causes an overwhelming feeling of anxiety and/or depression after you give birth to your baby. Many women wonder what causes postpartum depression and if there is anything they can do to prevent it. Postpartum depression does not occur because of something a mother does or does not do. The exact causes of postpartum depression are not well known—it is thought that it is caused by a combination of physical and emotional factors [2].
After giving birth, the levels of hormones, specifically estrogen and progesterone in a woman’s body quickly drop to almost nothing. This can lead to chemical changes in her brain that lead to a range of emotions like anxiety, insomnia, and depression. In addition to all the chemical changes new mothers face they are also dealing with sleep deprivation. Rest is vital in the postpartum period especially in helping to fully recover from childbirth. Sleep deprivation, stress, and the role of a new mother can lead to exhaustion, which can contribute to the symptoms of postpartum depression.
Sometimes a mother can feel like they will be looked down on if she expresses how she feels. Women often think this will reflect their ability to be a good mother. The woman will still take fabulous care of their family and this is why it is known as the “unknown/undiagnosed illness.” Postpartum depression can be debilitating and in severe cases lead to death. Today, there are wonderful treatment programs and support groups to help a woman know that they are not alone! Women should never feel embarrassed or ashamed of these feelings—there are many women facing this illness. Recently, a young mother of five children, Emily Dyches, lost her life from the complications of postpartum depression and anxiety. Her husband, Eric Dyches, started a wonderful non-profit organization titled, “The Emily Effect” [3]. This is a great resource to visit.
Your midwife will also be performing routine screening test before, during, and after pregnancy. Signs and symptoms of postpartum depression are listed below:
- Feeling agitated, hopeless, empty, or overwhelmed
- Insomnia, feeling tired but not being able to sleep
- Oversleeping, the constant feeling of being tired
- Irritability, feeling moody, or restless
- Anger, you might lose your temper easily, or feel like you don’t have control of your emotions
- Panic attacks, constantly worrying about situations you are brainstorming in your head
- Thinking about hurting yourself or your baby
- Excessive worrying
- Weight loss, loss of appetite
- Loss of interest in things you once enjoyed
- Women can feel disconnect from their infant or partner
Some important tips that could help you during this time include making sure you are getting enough rest, eating well, ask for help from family and friends, utilize support groups (online or in the community), exercise (even short walks can be beneficial), and do something that has made you happy in the past [5].
Please talk with your midwife if you are experiencing any of these symptoms, we LOVE you and are here to help you. You are not ALONE. Our emotional health is just as important as our physical health. Emotional + physical health are intertwine. Together we can overcome this disorder by effective treatment options and support groups catered for postpartum depression. #youarestrong

Resources
- https://womensmentalhealth.org/specialty-clinics/postpartum-psychiatric-disorders/?doing_wp_cron=1486164654.8663740158081054687500
- https://www.nimh.nih.gov/health/publications/postpartum-depression-facts/index.shtml
- http://theemilyeffect.org/
- http://www.postpartumprogress.com/ppd-support-groups-in-the-u-s-canada
- http://onlinelibrary.wiley.com/doi/10.1111/jmwh.12144/pdf

Breastfeeding

You finally have your baby in your arms and they are rooting (looking for the breast). You have always planned to breastfeed but this is harder than you thought and your baby is having a hard time latching. Just remember it will get better with each feeding, with each day, and by the time your baby is a month old they will be nursing like a pro. Don’t give up!
Research has shown that mothers who have a lot of support or have had an immediate family member breastfeed are more likely to breastfeed for at least 6 months and in may cases 1 year or more [1]. Your midwife is here to support you every step of the way. Please, if you are having a hard time and your baby is not picking it up like you thought they would, call your midwife! She or he will give you resources and put you in contact with a nurse specialized in providing breastfeeding support. You can do it!
Your nipples will be sore at the beginning but once the baby learns how to latch effectively the soreness will disappear and breastfeeding will become second nature. Below are signs of a good latch
- Most of the areola will be inside the babies mouth (at least 1 inch radius)
- You will see your baby’s ear wiggle
- There is circular movement of the jaw rather than rapid chin movement
- Your babies cheeks will be rounded
- You will not hear clicking or smacking noises, instead you will hear swallowing
- Your baby’s chin is touching your breast
- When your baby comes off the breast, the nipple is not flattened or misshaped
- Any discomfort ends quickly after getting the baby latched on
- Milk should not leak between the corners of the baby’s mouth
- Your baby ends the feeding with signs of satisfaction
- Signs of satisfaction include your baby looking relaxed, falls off the breast, has open hands, or falls asleep after [1]
Another worry of nursing mothers is that their baby is not getting enough to eat. It’s important to remember that breast milk is denser than formula so the amount of breast milk will be less than the amount of formula. You will know baby is getting enough if they have 4-6 wet diapers a day and 2-3 yellow colored poopy diapers a day. The good news is breast milk is a natural laxative, so some babies will have a poopy diaper with each feeding [6].
Warning signs
Sometimes a mother can develop a clogged milk duct that can lead to a breast infection called “mastitis.” A clogged milk duct develops when milk flow is blocked in a small area of the breast. Usually it has a gradually onset and only happens to one side of the breast. Signs of a clogged milk duct include the following:
- You will notice a hard lump area of engorgement
- Your breast will be swollen, bright read, and warm to the touch
- You will notice pain or tenderness on the affected breast
- Your milk let down will be painful and nursing on that side will be painful
It’s important to continue to nurse on that side even if it is painful. A clogged milk duct is caused from restricted milk flow. You may have skipped a feeding or become engorged and your breast was not emptied. Putting pressure on the duct can also cause restrict milk flow—maybe from a tight bra, sleeping on your stomach, or pressure from a strap on a diaper bag. Try taking ibuprofen (800 mg) to help with inflammation, make sure you are drinking plenty of fluids, and getting an adequate amount of sleep.
Mastitis is another infection that can happen while nursing. This can be caused by an infection, milk obstruction, or an allergy. Sometimes this infection can start from a cracked nipple. You are also at higher risk of developing it if you have a previous history of mastitis. This infection is most common in the first 2-3 weeks after the birth of your baby but can happen at any time while you are nursing. Mastitis usually has a sudden onset. Signs are similar to a clogged milk duct and listed below.
- The first sign is flu like symptoms, body aches, fatigue, nausea
- You can experience a fever that is greater than or equal to 100.4 F
- Your breast will be very painful
- Your breast can be hot, bright red, and swollen
- In some cases you will notice a red streak extending outward from the affected area
Just like with a clogged milk duct it’s important to continue to nurse on the affected side, even if it is painful. Heat can also help with the pain and encourage emptying of the breast. Use a warm compress and gentle massage to your breast before you nurse. Ensure you are getting enough rest and drinking enough fluids. Most importantly, make sure you are emptying your breast often, continue to nurse frequently and if you need too, use a breast pump. If symptoms of mastitis are mild and have been present for less than 24 hours, consider effective milk removal and supportive measures like ibuprofen (800 mg), warm compresses, and rest. If symptoms are not improving within 12-24 hours or if you are acutely ill, antibiotics should be started [2]. Call your midwife if you have any questions and she can guide you through treatment.
Lastly, don’t forget to take care of yourself while you are breastfeeding. You might feel extra hungry while you are breastfeeding, this is because your body is working around the clock making that precious breast milk. During pregnancy it is recommended to increase your caloric intake by 300 calories….well during breastfeeding you should increase your caloric intake by 500 calories. Your body will let you know when you are hungry and try to choose healthy items. If you get an intense craving (cravings can still happen during breastfeeding) listen to your body and just remember those sugaring cravings are OK in moderation. Below are some additional resources to help you during your breastfeeding journey and don’t forget to call the midwife if you have any questions.
Resources
- https://www.cdc.gov/breastfeeding/pdf/BF-Guide-508.PDF
- http://www.bfmed.org/Resources/Protocols.aspx
- Got Mom: http://www.gotmom.org/
- Le Leche League: http://www.llli.org/
- International Lactation Consultation Association: http://www.ilca.org/
- Breastfeeding website: http://www.breastfeeding.com/

Sexual intercourse after birth
Let me guess what you are thinking…sex is the last thing on your mind right now. Well I’m here to tell you that is completely OK. You can began sexual intercourse again when YOU feel YOU are ready, this choice should be completely individualized. The best thing to do is just have good communication with your spouse about your feelings and if the pain/tenderness doesn’t improve, call your midwife.
Current guidelines recommend waiting 4-6 weeks to resume sexual intercourse after having a baby. Some women feel ready to resume sex within a few weeks of giving birth, some women feel like they need a few months or longer. Orgasm for women is extremely mental—things like fatigue, stress and fear of pain all can take effect on your sexual desires.
Breastfeeding can also take a toll on your sex drive. The hormonal changes involved in nursing can lead to vaginal dryness and make it very tender. Perineal lacerations can also make sex very painful postpartum. Depending on the extent of your tear—you might need a couple months to heal. The most important thing to remember is that you can resume sexual activity when YOU feel ready. It will be painful the first attempt but should get better and better. Please call your midwife if the pain is not decreasing or if sexual intercourse is too painful to resume after a couple months.
Important things to consider
Take it slow, don’t jump right into it—start with cuddling or kissing. Ask your partner to give you a nice massage. If you are breastfeeding make sure you use a water-based lubrication. This will help tremendously with vaginal dryness, a side effect of breastfeeding. Try different positions to alleviate pain. This can take pressure off certain areas in the vagina and control the ease of penetration. Try to stay in the moment (women are use to multi-tasking) try only to think about the intimacy you are sharing with your partner. Avoid thinking about dirty diapers, the pile of laundry, or your never ending to do list. Easier said than done, I know:)!
Before sexual intercourse try taking a warm bath, consider taking ibuprofen, and make sure to empty your bladder. If sex is too painful to resume that is OK. There are plenty of alternatives like oral or manual stimulation. Just make sure to communicate with your partner what feels good and what doesn’t! Remember you might need more time to heal and that is totally fine.
Kegel exercises
After childbirth our pelvic muscles can lose their tone but don’t worry this is only temporarily. Decreased muscle tone can lead to decreased arousal during sex. To help tone that pelvic floor you can try something called “kegel exercises.”
The first thing you do is tighten your pelvic muscles. Think of this as the feeling of stopping urine midstream. Tighten those muscles and hold for 10 seconds, release for 10 seconds, and than hold those muscles again for 10 seconds. After you get it down try holding for 15 seconds and than 20 seconds. Pretty soon your pelvic muscles will be back up to par. Try to do at least 3 sets of 10 during the day. You can do this while you are driving, lying in bed, or even while you are vacuuming. This will help tone up your pelvic floor and prevent incontinence that can happen later in life after childbirth.
Remember to talk to your midwife if sexual intercourse continues to be painful. Your midwife can discuss numerous treatment options with you. Intimacy is a healthy part of your relationship and you should be able to enjoy sex again after giving birth. Many women believe that painful intercourse is the result of having a vaginal birth. This is a misconception. You can enjoy sex before, during, and after pregnancy. Remember you can get pregnant while breastfeeding so ensure you have adequate contraception before resuming sexual intercourse.
Resources

Positions During Labor
 Recently, a woman explained that during delivery of her baby she pushed for 3.5 hours on her back, in the “dorsal lithotomy” position, using an epidural for pain relief. Dorsal lithotomy means the woman is laying on her back with her legs in stirrups. She explained that she was diagnosed with “failure to progress” and this resulted in an emergent cesarean. Now there is no saying for 100% sure that if she changed positions the baby would have been born vaginally but I will say that I have witnessed the many benefits of position changes. Frequent position changes during pushing helps the baby engage and move down into the mother’s pelvis. Some positions can open the mothers pelvis 20-50% more making it easier for the baby to be born.
Recently, a woman explained that during delivery of her baby she pushed for 3.5 hours on her back, in the “dorsal lithotomy” position, using an epidural for pain relief. Dorsal lithotomy means the woman is laying on her back with her legs in stirrups. She explained that she was diagnosed with “failure to progress” and this resulted in an emergent cesarean. Now there is no saying for 100% sure that if she changed positions the baby would have been born vaginally but I will say that I have witnessed the many benefits of position changes. Frequent position changes during pushing helps the baby engage and move down into the mother’s pelvis. Some positions can open the mothers pelvis 20-50% more making it easier for the baby to be born.
Did you know you can still change positions in bed with an epidural? Just ask to have your epidural low dosed so you can still move your legs. How cool is that? After all, women were not meant to have babies on their back in bed. If you decide you want to go natural you will learn that it is very uncomfortable to be in bed on your back during active labor. Not to mention changing positions acts as pain relief, helps the baby move down and engage in the pelvis, and it helps labor progress by utilizing gravity and helping the mother relax. Don’t worry your midwife has you covered—she is trained not only to provide you with support during labor, she can deliver your baby in almost any position that is comfortable for you.
The following labor positions can be used during labor to act as pain relief + open up the mother’s pelvis:
- Squatting: Squatting helps widen the pelvic opening for baby to come out. It relieves back pain, it speeds up labor, relaxes the perineal muscles so you are less likely to tear, and improves oxygenation to the baby. It also helps promote delivery of the placenta after the birth of your baby. Practice this position during your pregnancy. Remember it can help open up your pelvis 20-30% more, making it an easy pathway for baby.
- Hands and Knees: This position looks how it sounds. The laboring mother kneels on both knees and leans forward onto her hands or leans on other support devices like pillows or a birthing ball. Personally, I have found that the woman loves the lean over the birthing ball as it helps her relax. You can do this position on the floor if you have a soft surface like carpet or a yoga mat or it can be done in a bed. This position is very comfortable for a mother going natural but it can also be done if the mother has an epidural—as long as she has excellent support from a doula, nurse, and midwife.
- Side lying: In this position you can lie on your left or right side. Your body is supported with at least five pillows—one or two under your head, one supporting your top knee, one behind your back, and another under the abdomen bulge. This position can be helpful when the mother is tired and needs a rest from being upright. This position can also be done with and without an epidural. This birthing position is very effective for maintaining relaxation. The woman is able to reduce unnecessary muscular effort….this results in less fatigue during a long labor and greatly increases her comfort level.
- Dorsal lithotomy: This is one of the most common birth positions in a hospital. In this position the woman li
 es flat on her back or at a slight incline with her legs in stirrups. There really are no advantages to this position other than it doesn’t interfere with the urinary catheter, IV line, or fetal monitoring system. It also provides an easy access to the perineum for healthcare providers. If you want to avoid tearing, you want to avoid this position. This position also results in the narrowest pelvic opening and puts pressure on the coccyx. This position increases the need for vacuum and forceps delivery. The woman has to push against gravity in this position. It also increases the risk of having a malpositioned baby resulting in a slower progression of labor.
es flat on her back or at a slight incline with her legs in stirrups. There really are no advantages to this position other than it doesn’t interfere with the urinary catheter, IV line, or fetal monitoring system. It also provides an easy access to the perineum for healthcare providers. If you want to avoid tearing, you want to avoid this position. This position also results in the narrowest pelvic opening and puts pressure on the coccyx. This position increases the need for vacuum and forceps delivery. The woman has to push against gravity in this position. It also increases the risk of having a malpositioned baby resulting in a slower progression of labor.
It’s important to remember there is definitely more than one position you can try during labor and your midwife will help you change positions frequently. Listen to your body and try to practice these positions during your pregnancy. Request for frequent position changes while you are pushing—this can be done with and without an epidural. Now you are on your way to a positive birth experience.
Intermittent Auscultation
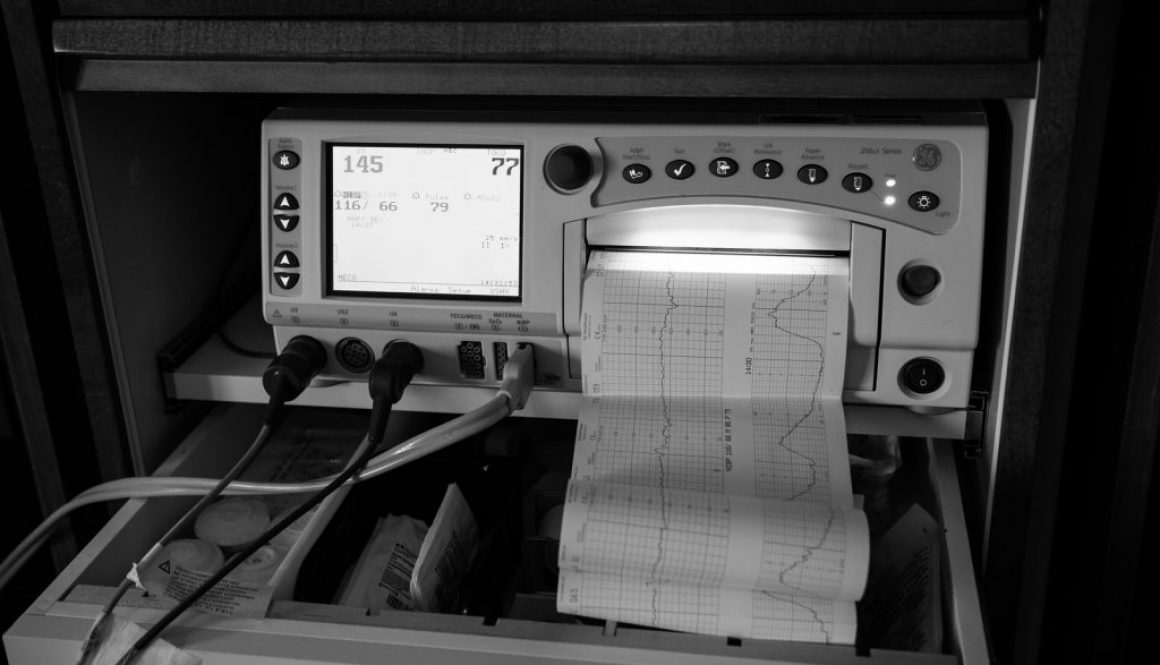
 Continuous monitoring (also known as external fetal monitoring) of your baby’s heart rate during labor is the standard of care in hospitals throughout the US today. It is important to understand that there are risks and benefits for continuous monitoring. Continuous monitoring is required during labor induction to ensure your baby is tolerating labor ok. Continuous monitoring is also required if you decide to get an epidural or during the administration of any pain medications.
Continuous monitoring (also known as external fetal monitoring) of your baby’s heart rate during labor is the standard of care in hospitals throughout the US today. It is important to understand that there are risks and benefits for continuous monitoring. Continuous monitoring is required during labor induction to ensure your baby is tolerating labor ok. Continuous monitoring is also required if you decide to get an epidural or during the administration of any pain medications.
It is important to note that continuous monitoring is associated with an increased risk of unnecessary cesareans [1]. Research has found that there is no decrease in fetal death or incidence of cerebral palsy with external fetal monitoring. Cerebral palsy is a disease that was originally thought to be caused from lack of oxygen during delivery. If we cannot prevent this disorder with external fetal monitoring, why is it the standard of care? Liability is a big concern for healthcare providers today. A big increase in lawsuits against providers who delivered a child vaginally that later turned out to have cerebral palsy have increased the use of external fetal monitoring [1].
 Many studies have shown that a decrease in heart rate of the fetus during labor and delivery are more often the result of a reflex response to changes in the baby’s circulation and such drops are normal and can do relatively little or no harm [1]. Today, we know that cerebral palsy is not caused by a lack of oxygen during delivery. Instead, birth defects, growth restriction, infections, inflammation and other unidentified factors can cause the condition [2].
Many studies have shown that a decrease in heart rate of the fetus during labor and delivery are more often the result of a reflex response to changes in the baby’s circulation and such drops are normal and can do relatively little or no harm [1]. Today, we know that cerebral palsy is not caused by a lack of oxygen during delivery. Instead, birth defects, growth restriction, infections, inflammation and other unidentified factors can cause the condition [2].
It has been found that fetal monitoring strips read by experienced obstetricians tend to interpret the monitor reading very differently [1]. In fact, when an obstetrician was allowed to evaluate the same reading twice several months apart, the interpretation differed even more. It’s easy to interpret a good fetal heart rate tracing (cat. I) verses a bad tracing fetal heart rate tracing (cat. III) but everything in between (cat. II) can be very tricky. This type of inconsistency has made the United States Preventive Services Task Force rate electronic fetal monitoring as having the lowest grade of effectiveness possible [4]. So if you don’t want to be tied down to the bed during labor or if the monitoring device is bothering you, ask your midwife about intermittent auscultation. If you have had an uncomplicated pregnancy and are planning to have a natural birth this is likely an option for you [1].
What is intermittent auscultation?
Intermittent Auscultation is a method of listening to fetal heart tones with a fetascope (like a stethoscope) or a hand-held ultrasound device (doppler). During intermittent auscultation your midwife will listen closely to rate, rhythm, and variability of your baby’s heart rate for at least one full minute before, during, and after a uterine contraction. This process gathers information that is charted by your midwife to represent a baseline rate, presence or absence of accelerations, decelerations, and the presence or absence of variability. The purpose is to ensure the midwife in making information-based, logical management decision during labor and birth of your baby. Intermittent auscultation protect the well being of your unborn baby without exposing the mother to the risks of unnecessary interventions [2].
Using intermittent auscultation you can expect your midwife to listen to your baby’s heart rate every hour during the early phase of labor, every 30 minutes when you are actively laboring, and every 15 minutes while you are pushing. This provides the ability to move freely around during labor and not have devices on your abdomen that can be uncomfortable or irritating.
Remember that the goal of a midwife is to give you the information for you to make an informed decision. It is always your CHOICE what route you decide to go. If you are looking for a low intervention, natural approach, talk to your midwife about intermittent auscultation. Below are a list of links that provide more resources about external fetal monitoring and intermittent auscultation.
Resources
- https://cerebralpalsynewstoday.com/2016/12/09/electronic-fetal-monitoring-no-benefits-plenty-of-harm
- http://birthtools.org/Reducing-Primary-Cesareans
- http://onlinelibrary.wiley.com/doi/10.1016/j.jmwh.2010.05.007/full
- https://www.uspreventiveservicestaskforce.org

What is a doula?
 A doula is a trained professional who provides continuous physical, emotional, and informational support to a mother before, during, and shortly after childbirth to help her achieve the healthiest, most satisfying experience possible [1].
A doula is a trained professional who provides continuous physical, emotional, and informational support to a mother before, during, and shortly after childbirth to help her achieve the healthiest, most satisfying experience possible [1].
Countless studies have investigated doula care and have shown the improved physical and physiologic outcomes for both mother and baby. Doulas have a positive impact on not only the mother but also the entire family. Research has shown that women who use a birth doula are less likely to need Pitocin, less likely to have a cesarean birth, less likely to use pain medications, and more likely to rate their childbirth experience as positive [1].
Doulas offer physical support, emotional support, partner support, evidence-based information, and advocacy. They provide resources to help the mother ask her midwife great questions in helping her make informed decisions about her pregnancy. Doulas help bridge the gap of communication between women and their midwife, lifting them up to help them find their voices and advocate for the very best care [2].
Midwives love and respect doulas. They value their care and highly recommend their services to all pregnant women. Ask your midwife about local organizations and different doula groups she recommends in your area. Some hospitals have volunteer doula programs that provide doula services at no charge. You can’t go wrong with a doula. Below are some more resources.
Resource
1. Find a doula: www.dona.org
2. Doula World: www.doulaworld.com

Eating healthy during Pregnancy
 I’m sure you have heard how important it is to eat healthy during your pregnancy–but what exactly is healthy? Well I am here to tell you! Hopefully you will learn of food options that include those vital vitamins and minerals that are essential during pregnancy.
I’m sure you have heard how important it is to eat healthy during your pregnancy–but what exactly is healthy? Well I am here to tell you! Hopefully you will learn of food options that include those vital vitamins and minerals that are essential during pregnancy.
It is recommended to consume 75 grams of protein daily during your pregnancy…..75 grams! This might seem like a lot but you will be surprised just how easy it is. The following list contains foods high in protein that might sound good to you.
Eggs (6 grams per egg)
Chicken Breast (43 grams per breast)
Cottage Cheese (25 grams in 1 cup)
Milk 2% (8 grams in 1 cup)
Greek Yogurt (23 grams in 1 cup)
Steak (23 grams per 3 oz. serving)
Peanut butter (8 grams per 2 tbsp)
Mixed Nuts (6 grams per 2 oz.)
After all your body is creating a human, a healthy nutritious diet is key. Don’t forget to include other vital vitamins and minerals for all those cells that are multiplying quickly. Let’s talk about iron; during pregnancy your blood volume increases by 50% to support the needs of you and your baby. It can be common for women to develop anemia. Midwives will recommend taking iron supplements if your Hematocrit is less than 33% or you hemoglobin is less than 11 g/dL, these values are found in a blood test called complete blood count (CBC). Your midwife will talk with you about your results. Sometimes our body doesn’t absorb iron supplements very well. Some studies have shown that iron absorption is best when it is consumed in your diet. The American Academy of Obstetrics and Gynecology recommends taking vitamin C with iron to help with absorption [1]. Try taking a glass of orange juice in the morning with some iron-fortified cereal. It is recommended to consume 27 mg of iron daily during pregnancy. Foods that are high in iron include:
Spinach (3-12 mg per 1/2 cup)
Fortified cereals (3-12 mg per 1 cup)
Liver (12 mg per serving)
Beef (3-12 mg per serving)
Beans (7 mg per 1 cup)
Lentils (6 mg per 1 cup)
Chickpeas (5 mg per 1 cup)
Chicken breast (5 mg per 1 cup)
Dried apricots (3.5 mg per 1 cup)
Calcium intake is also very important. It ensures your baby develops strong bones, teeth, heart, nerves system, and muscles. Some studies have also shown that it can help prevent preeclampsia. With those results you want to ensure you are consuming enough. It is recommended to consume 1,000 mg of calcium daily. The following foods are high in calcium:
Milk (300 mg per 1 cup)
Yogurt or Kiefer (300 mg per 6 oz or 3/4 cup)
Cheese (224 mg per 1 oz)
Broccoli (93mg per 1.5 cups)
Almonds (75 mg per 1 oz)
Orange juice (75 mg per 1 cup)
Kiwi (60 mg per 1 cup)
Dried Apricots (5 mg per apricot)
Folic acid is also important. This B vitamin prevents birth defects in the baby’s brain and spine also known as “neural tube defect.” You should consume at least 600 mcg daily during pregnancy. This amount is usually found in the standard prenatal vitamin. There is controversy about how much of the prenatal vitamin our body actually absorbs so consider the food sources listed below.
Spinach (263 mcg per 1 cup)
Romaine Lettuce (75 mcg per 1 cup)
Broccoli (52 mcg per 1/2 cup)
Asparagus (262 mcg per 1 cup)
Oranges (40 mcg per 1 cup)
Black Beans (256 mcg per 1 cup)
Pinto Beans (294 mcg per 1 cup)
Peanuts (88 mcg per 1/4 cup)
And don’t forget to drink, drink, drink–drink water that is. During pregnancy you should be drinking at least 10, 8 oz glasses of water a day or 2 liters. Carry around that water bottle mamma, you will feel better and have more energy. Even though you might be using that energy to walk to the bathroom:).
Foods to Limit
Perhaps one of the most confusing food items during pregnancy is fish! Some fish is very healthy and recommended during pregnancy, like salmon for example. Other fish that is high in “methyl mercury” you should avoid! Fish that contains high amounts of mercury that should be avoided include swordfish, shark, king mackerel, ahi tuna, and marlin. It is recommended to consume no more than 2-3 servings of fish per week. Good options that are a good source of protein include salmon, canned tuna, cod, and tilapia. Remember don’t exceed 2-3 servings per week.
Caffeine…..how will you live 9 months without coffee or soda? The good news is you can still have caffeine and soda, just try to limit your amount. During pregnancy you should not have more than 2 servings of caffeine per day or 200 mg per day. This includes all drinks like soda, tea, and coffee. 12 oz of coffee contains 200 mg of caffeine, so just be aware that if you have coffee you should probably avoid tea and soda. Try to substitute these drinks for water or milk. If you can try to avoid caffeine but studies have shown that small amounts are OK during pregnancy.
Don’t forget to limit the foods you consume that are high in fat, sugar, grease, and oil. Pregnancy cravings are real so if something sugary sounds good or maybe something greasy, you can go with your cravings but just remember to limit your amount. Don’t make it a daily habit and maybe go for an evening walk after you fix that craving. All in moderation right?:)
Foods to Avoid
During pregnancy it recommended to never consume alcohol, alcohol in the mother’s blood can pass directly to the baby’s blood and cause fetal alcohol syndrome. This disorder can lead to severe learning disabilities and behavioral problems. If you are having problems avoiding alcohol please talk with your midwife, we are here to help you and your unborn child. Remember that there will never be judgment but rather a specialized plan to help you and your baby.
Avoid raw or undercooked meats. Toxoplasmosis is a serious infection found in raw/undercooked meats. Toxoplasmosis can pass directly to your baby and cause blindness or mental retardation. You should also avoid raw fish, ensure meat is cooked thourougly before consuming.
Unpasteurized foods should also be avoided. They have the potential for spreading listeria. Listeria infections can cause preterm labor, miscarriage, and stillbirth. Well what is unpasteurized foods? It can be unpasteurized milk or delicate cheeses made from unpasteurized milk. These include brie, feta, queso blanco, or blue-veined cheeses. Food becomes pasteurized when it is heated up to high temperatures to kill harmful bacteria. It is also recommended not to have hot dogs, lunchmeat, or any seafood salads that haven’t been warmed up first. Talk with your midwife if you have any concerns, she can help you modify your diet so if fits the nutritional demands of pregnancy.
Resources
- http://www.acog.org/Patients/FAQs/Nutrition-During-Pregnancy
- http://onlinelibrary.wiley.com/store/10.1016/j.jmwh.2009.08.019/asset/j.jmwh.2009.08.019.pdf?v=1&t=iz91n86e&s=b234eddce10f6126df4dba8ef46958ab490b1e86
